Expedite Your Billing Processes
While Electronic Remittance Advice (ERA or 835) files have expedited the billing process for most providers and payers, they have complicated some of the secondary billing and revenue cycle management tasks.
Freedom Imaging Systems' FreeX12 Processor shortens the billing revenue cycle by processing the raw 835 Health Care Claim Payment/Electronic Remittance Advice files and providing readable electronic images in both batch and patient centric formats. FreeX12 then places the correct patient centric claim in denial/reason code specific workflow queues.
FreeX12 Processor presents 835/ERA files in a digital, human-readable EOB-like (Explanation of Benefits) statement. Information within 835/ERA files is captured and then presented at two different levels — batch and patient. At the batch level, information is automatically indexed by numerous fields including payment date, payment method, check number, check amount, payer name, provider name, provider number, etc.
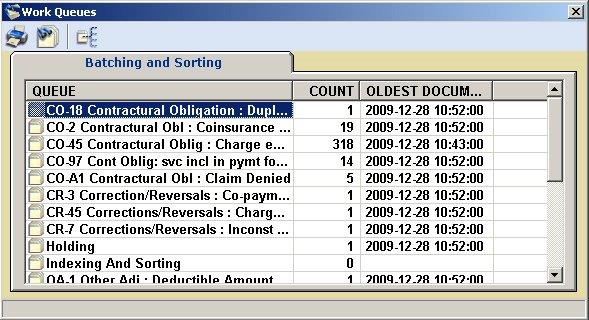
At the patient level, information from the electronic file is displayed for each individual patient. It too is indexed and searchable by fields such as payment date, patient's first and last name, subscriber ID, patient account number, etc. Not only is each patient remit easy to search and find, but it is also displayed individually. Denials are automatically placed into workflow queues based on denial/reason codes, thus automating working denials. The amount of time saved by the functions of FreeX12 processor will reduce processing time for secondary and tertiary billing.
RICAR can be installed in a variety of ways. Traditionally it is installed on-premises via a LAN, WAN, or VPN connection. RICAR installation is also available via Freedom's SAS 70 certified Cloud network.
Most importantly, you'll discover that FreeX12 processor decreases Days Sales Outstanding (DSO) for an easy to measure increase in revenue and return on investment (ROI).
Freedom's FreeX12 Processor speeds up 835 processing with:
- Prioritized patient centric denial/reason code processing for all payers.
- Claim specific images with denial /reason code glossary specific to the claim.
- Claim specific images distributed to billers electronically via workflow.
- Automatic secondary and tertiary processing.
- Claim specific printing for secondary billing, eliminating redaction.
- Fully searchable batch level viewing for balancing and reviewing.
- Fully searchable patient level viewing for researching and fast customer service.
For more information about how Freedom Imaging Systems can help expedite your billing processes call 734.327.5600 to speak to one of our representatives or click here to watch a demo
 734.327.5600
734.327.5600 Contact Us
Contact Us